Managing Type 2 diabetes has always required a vigilant approach, from monitoring blood sugar levels to keeping up with lifestyle changes and doctor’s visits. But, as healthcare becomes increasingly digitized, cellular remote patient monitoring (RPM)™ offers a promising solution to make diabetes management more accessible, effective, and personalized. Embracing cellular RPM can be a game-changer for managing Type 2 diabetes. By using cellular RPM, patients and their healthcare providers can gain real-time insights into health data, allowing for timely adjustments that can drastically improve outcomes.
Understanding Remote Patient Monitoring for Diabetes Management
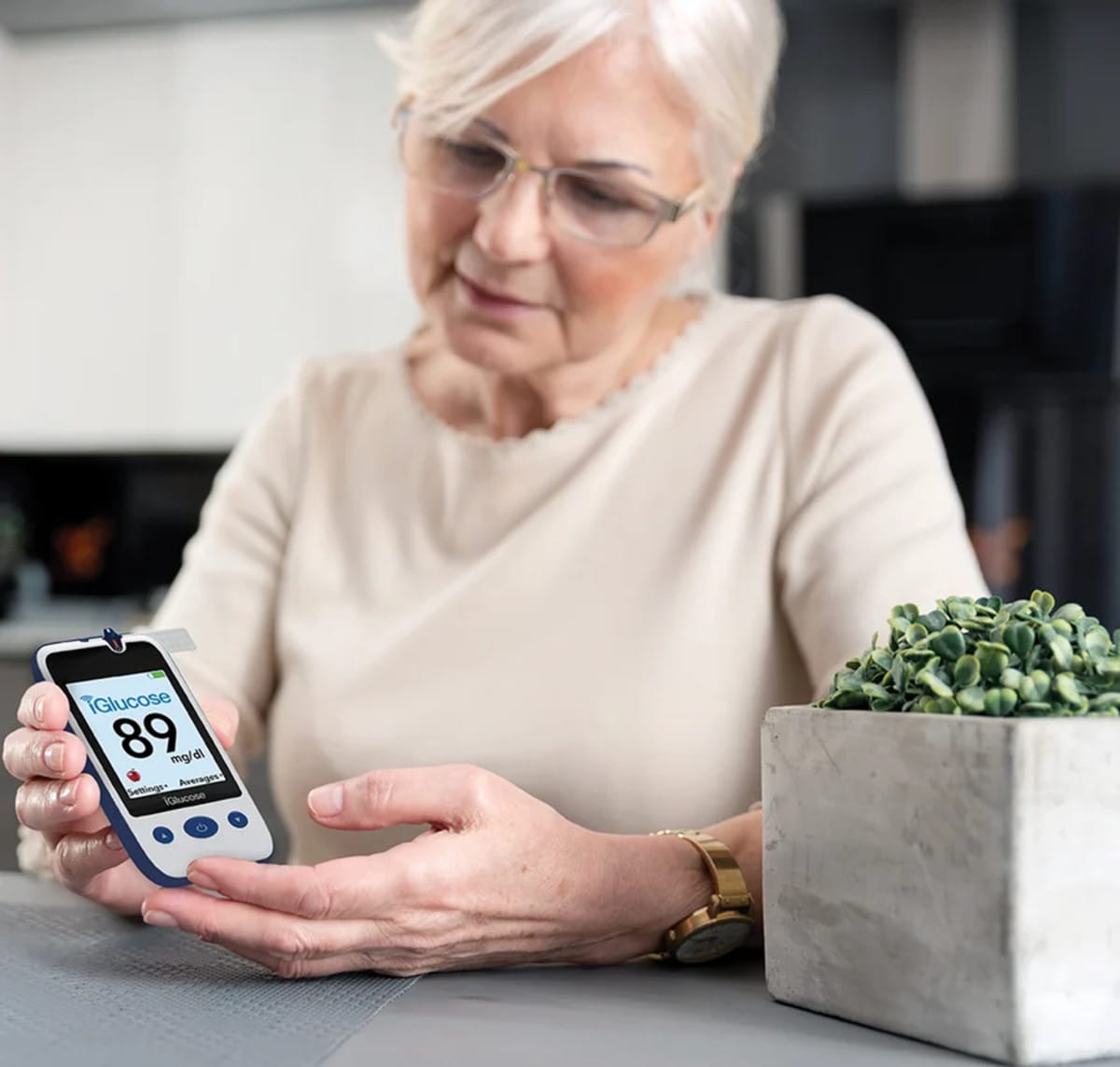
Remote Patient Monitoring (RPM) involves using digital devices like glucose meters and connected blood pressure monitors that transmit data directly to healthcare providers. With RPM, data on vital health indicators can be captured consistently in a non-intrusive way.
For diabetes management, cellular RPM is particularly valuable because it allows patients to monitor essential data, including blood glucose levels, heart rate, and other vital signs. Providers can view this data in real time, allowing them to make informed decisions on medication, dietary plans, and lifestyle modifications much faster than waiting for a regular office visit.
Why Cellular RPM is Effective for Managing Type 2 Diabetes
Type 2 diabetes management is highly individualized and requires continual monitoring to prevent complications. Cellular RPM provides significant advantages in this regard:
- Consistent Data Collection: Instead of relying on occasional glucose readings, cellular RPM gives a more comprehensive view of glucose patterns. With regular testing, this consistent data can help both patients and doctors identify trends and make proactive adjustments to avoid blood sugar spikes or drops.
- Immediate Feedback: Traditional methods of diabetes management often depend on periodic doctor visits. Cellular RPM can provide immediate feedback to the patient and the provider, enabling timely interventions that can prevent worsening symptoms and long-term complications.
- Personalized Health Insights: Every person with diabetes has unique responses to medication, diet, and exercise. Cellular RPM data allows for highly personalized recommendations, which can optimize treatment plans and improve overall management of the condition.
- Convenience and Accessibility: For those with limited access to regular healthcare due to location, mobility issues, or time constraints, cellular RPM eliminates barriers to receiving continuous care. Cellular monitoring devices allow patients to perform routine vital sign tests from the comfort of their home, reducing the need for frequent clinic visits.
Benefits of Cellular RPM for Patients with Type 2 Diabetes
Here’s how patients with Type 2 diabetes can benefit from cellular RPM in their daily lives:
- Enhanced Self-Management: Cellular RPM encourages patients to become more proactive in managing their diabetes. Real-time data empowers them to take immediate steps, when necessary, whether it’s adjusting their diet or being more physically active.
- Reduced Risk of Complications: With cellular RPM, doctors can detect alarming trends in health data before they become critical. Early intervention can significantly reduce the risk of complications such as neuropathy, retinopathy, cardiovascular diseases, and kidney damage.
- Mental Health Support: Managing diabetes can be stressful and overwhelming, often leading to burnout or even anxiety. By offering consistent feedback and a sense of control, cellular RPM can reduce mental strain, helping patients feel more in control of their health and less burdened by the condition.
- Improved Patient-Doctor Relationship: cellular RPM enables a collaborative approach where patients and healthcare providers work as a team, with open channels of communication. This dynamic exchange fosters trust, and patients are more likely to adhere to treatment plans when they feel supported.
How to Get Started with Cellular RPM for Diabetes Management
- Consult A Healthcare Provider: The first step for patients who want to begin using cellular RPM for diabetes management is to consult a doctor. Most physicians are familiar with RPM and should be able to provide options for the right solutions based on individual health needs.
- Choose the Right Technology: There are only a few cellular RPM devices specifically for diabetes management. The physician should recommend a device that is compatible with their system or work with an RPM/CCM system partner to ensure seamless data sharing.
- Set Goals and Stick to a Routine: Cellular RPM is most effective when it’s consistent. With some cellular RPM glucose meters, the physician can set reminders for patients, so they know when they are supposed to test as recommended. By doing this, consistent testing should eventually become a part of the patient’s daily routine.
- Be Prepared for a Learning Curve: Like any technology, cellular RPM tools may take time to get used to. Everyone involved should be prepared to assist others with the learning process.
- Review and Examine Data Thoroughly: Cellular RPM only works if the insights it provides are reviewed and utilized to improve a patient’s health. Pay attention to the patterns in the data, note any changes and communicate with the patient when there is a concerning trend. The data is there to empower change and improve a patient’s health.
Cellular RPM can be a Long-Term Solution
Managing Type 2 diabetes is typically a lifelong journey, but cellular RPM can provide a new path to make the trip a little easier and has been proven to improve outcomes. Using a cellular RPM is not just about helping patients track glucose levels, but it allows them to take a proactive step toward preventing complications and achieving optimal health. Studies have shown that cellular RPM users often see improvements in glycemic control, decreased hospitalization rates, and better overall quality of life.
A Howard University study of patients with diabetes using the iGlucose®, resulted in 70% of high-risk participants lowering their A1c by an average of 2.8% within 90 days1
A 30-day study2 by the University of Arkansas for Medical Sciences of 59 pregnant women with Type 1 or Type 2 diabetes, who frequently tested with Smart Meter’s cellular-enabled iGlucose® glucometer showed an increased satisfaction with their diabetes management. Eighty-six percent of participants noted that the automatic transmission of blood glucose results to their physician helped them better maintain their condition.
Baum Consulting Services implemented an RPM program3 using Smart Meter’s cellular iGlucose and saw excellent results. One patient with diabetes had an A1c of 10.4 before starting the program but was able to reduce that to 6.6 in about a year and a half on the RPM program.
In a recent survey4 of more than 200 people with Type 2 diabetes, the overwhelming majority (88%) said they would test their glucose more consistently if they knew the reading was being sent to their provider. And that number increased 27% compared to the percentage (61.5%) that answered that way to the same question in the 2023 survey.
Conclusion
Cellular RPM has the potential to transform diabetes care by allowing patients and providers to stay connected and engaged in real-time. For those living with Type 2 diabetes, RPM can make daily management more efficient and less stressful, helping patients lead healthier, more empowered lives. As healthcare technology continues to evolve, embracing RPM is a forward-thinking decision that makes diabetes management smarter and more sustainable.
With RPM, controlling Type 2 diabetes doesn’t have to feel like a full-time job. It’s a powerful ally that can support patients on their path to better health and long-term well-being.
1 – The Benefits of Remote Monitoring of Real Time Blood Glucose Data Using iGlucose System in Managing Patients with Diabetes, Howard University Diabetes Center.
2 - Use of Cellular-Enabled Glucometer for Diabetes Management in High-Risk Pregnancy - Jones RD, Peng C, Odom L, Moody H, Eswaran H (2023) Use of cellular-enabled glucometer for diabetes management in high-risk pregnancy, Telemedicine Reports 4:1, 307–316, DOI: 10.1089/tmr.2023.0033.